
Watch short for this article (5 slides)
Dengue Fever's Deadly Ascent: How Climate Change Fuels a Global Health Crisis
Dengue fever, a debilitating mosquito-borne viral illness, is no longer confined to tropical hotspots. Its geographic range and the intensity of outbreaks are expanding at an alarming rate across the globe, posing a rapidly escalating public health threat. While factors like rapid urbanization, increased global travel, and gaps in sanitation infrastructure contribute significantly, compelling evidence points to climate change as a powerful accelerator, amplifying the conditions that allow Dengue-carrying mosquitoes and the virus itself to thrive. Understanding the intricate links between our changing climate and Dengue's spread is critical for developing effective prevention and control strategies in an increasingly vulnerable world.

Decoding Dengue: The Virus, The Vector, and The Disease
Before exploring the climate connection, it's essential to understand the key players:
- The Virus (DENV): Dengue fever is caused by the Dengue virus, belonging to the Flaviviridae family. There are four distinct, but closely related, serotypes (DENV-1, DENV-2, DENV-3, and DENV-4). Infection with one serotype provides lifelong immunity to that specific type, but only temporary cross-immunity to the others.
- The Vectors: The virus is primarily transmitted to humans through the bites of infected female mosquitoes of the *Aedes* genus, mainly:
- Aedes aegypti (Yellow Fever Mosquito): Highly adapted to urban environments, prefers to breed in artificial containers (tires, buckets, pots), feeds almost exclusively on humans, and often bites multiple people during a single feeding cycle. It thrives in warm climates.
- Aedes albopictus (Asian Tiger Mosquito): More cold-tolerant than *Ae. aegypti*, allowing it to establish in temperate regions. It breeds in both artificial containers and natural habitats (like tree holes) and feeds on animals as well as humans, though it is generally considered a less efficient Dengue transmitter than *Ae. aegypti*. Its expanding range is a major factor in Dengue's spread to new areas.
- The Disease Spectrum: Dengue infection can manifest in several ways:
- Asymptomatic Infection: Many infections (up to 75% by some estimates) cause no noticeable symptoms.
- Undifferentiated Fever / Dengue Fever (DF): Characterized by sudden high fever (40°C/104°F), severe headache, pain behind the eyes, muscle and joint pains ("breakbone fever"), nausea, vomiting, swollen glands, and rash. Usually resolves within a week.
- Severe Dengue (Dengue Hemorrhagic Fever - DHF / Dengue Shock Syndrome - DSS): A potentially lethal complication, more common after a secondary infection with a *different* DENV serotype. Characterized by plasma leakage, fluid accumulation, respiratory distress, severe bleeding, or organ impairment. This phenomenon, potentially linked to Antibody-Dependent Enhancement (ADE) where pre-existing antibodies facilitate viral entry into cells, makes subsequent infections particularly dangerous. Prompt medical intervention is crucial. (WHO - Dengue and Severe Dengue Fact Sheet)
Climate Change as an Amplifier: How Weather Fuels the Fire
Climate change directly impacts the lifecycle, distribution, and behavior of *Aedes* mosquitoes and the replication rate of the Dengue virus within them, creating more favorable conditions for transmission:
1. Rising Temperatures: Expanding Horizons and Accelerating Cycles
- Geographic Range Expansion: Warmer temperatures allow *Aedes* mosquitoes, particularly the more cold-tolerant *Ae. albopictus*, to survive winters and establish populations in previously unsuitable temperate regions (e.g., Southern Europe, parts of the US). Average temperatures consistently above 15-18°C (59-64°F) become more conducive to their survival and activity.
- Faster Mosquito Development: Higher temperatures accelerate the mosquito lifecycle from egg to larva to pupa to adult, leading to larger mosquito populations more quickly.
- Increased Biting Frequency: Mosquitoes digest blood meals faster at higher temperatures, leading them to bite more frequently to produce eggs, thus increasing transmission potential.
- Shortened Extrinsic Incubation Period (EIP): This is a critical factor. The EIP is the time required for the Dengue virus to replicate within the mosquito after an infected blood meal, reach the salivary glands, and become transmissible. Higher temperatures significantly shorten the EIP (e.g., from ~12 days at 25°C to ~7 days at 28-30°C). A shorter EIP means mosquitoes become infectious faster, increasing the likelihood they will transmit the virus before they die. (CDC - Climate Change and Dengue Fever)
2. Altered Precipitation Patterns: Breeding Grounds and Drought Paradox
- Increased Rainfall & Flooding: Intense rainfall events, often associated with climate change, can create numerous temporary pools and fill artificial containers, expanding potential breeding sites for *Aedes* mosquitoes, especially in urban areas lacking good drainage. Post-flood environments often see surges in mosquito populations.
- Drought Conditions (The Paradox): Conversely, periods of drought can also increase Dengue risk. When regular water supplies are disrupted, people are more likely to store water in open containers (drums, tanks, buckets) around their homes, inadvertently creating ideal breeding habitats for *Ae. aegypti* close to human populations.
3. Higher Humidity: Enhanced Mosquito Survival
- Optimal humidity levels (generally moderate to high) increase the survival rate and activity levels of adult mosquitoes, extending their lifespan and providing more opportunities to bite and transmit the virus. Climate change influences regional humidity patterns.
4. Extreme Weather Events: Disruption and Displacement
- Hurricanes, floods, and other extreme events linked to climate change can disrupt public health infrastructure, hinder mosquito control efforts, displace populations (potentially introducing the virus to new areas), and create abundant breeding sites in the aftermath, often leading to outbreaks.
The Intergovernmental Panel on Climate Change (IPCC) explicitly notes the link between climate change and the expansion of vector-borne diseases like Dengue in its assessment reports.
Urbanization: A Breeding Ground Magnified by Climate
Rapid and often unplanned urbanization creates environments highly conducive to *Aedes* mosquitoes, synergizing dangerously with climate change:
- Abundant Breeding Sites: Dense housing, inadequate waste management (creating water-holding containers like tires and plastics), poor drainage, and reliance on water storage containers provide endless breeding opportunities for *Ae. aegypti*.
- High Human Density: Provides ample hosts for mosquitoes, facilitating rapid virus transmission within a community.
- Urban Heat Island Effect: Cities tend to be warmer than surrounding rural areas, further enhancing mosquito development and activity, especially when combined with background climate warming.
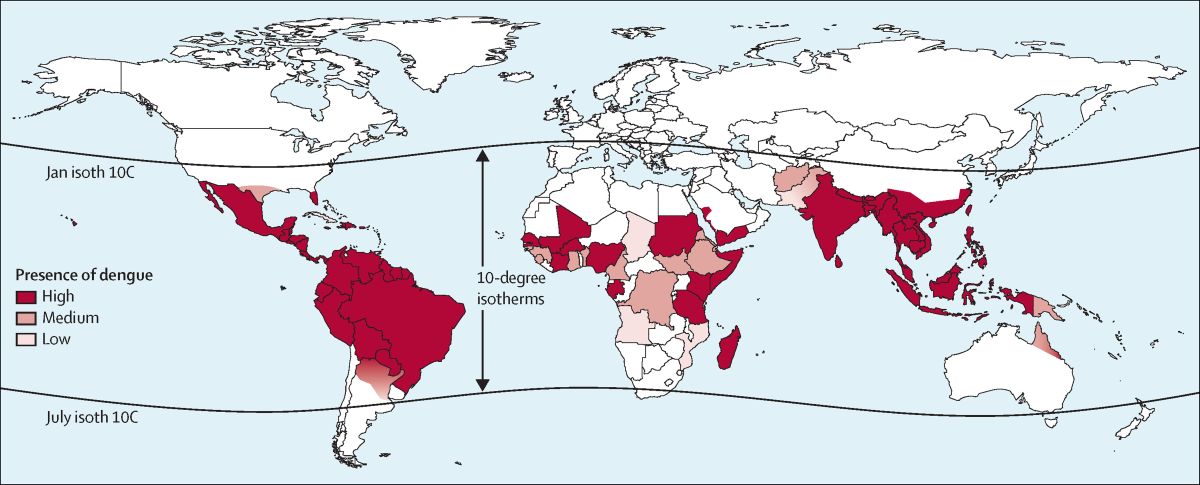
Mapping the Surge: Dengue's Expanding Footprint
Once primarily endemic to Southeast Asia and Latin America, Dengue's map is rapidly being redrawn:
- Hyperendemic Regions Intensifying: Countries like Brazil, Colombia, Peru, the Philippines, Thailand, and Vietnam face increasingly large and frequent outbreaks, straining healthcare systems. Brazil, for instance, has reported record-breaking case numbers in recent years.
- Emergence in New Territories:
- Southern Europe: Local transmission events, indicating established mosquito populations capable of spreading the virus, have been reported in France, Italy, Spain, and Croatia, linked to the expansion of *Ae. albopictus* facilitated by warmer conditions.
- United States: While imported cases are common, locally acquired Dengue cases (meaning transmission occurred within the US) have become more frequent in Florida, Texas, Arizona, and Hawaii, signaling the establishment of competent vectors and suitable transmission conditions.
- High-Altitude Areas: Dengue is appearing at higher elevations in countries like Nepal and Colombia, areas previously considered too cool for sustained transmission.
Fighting Back: Integrated Strategies in a Warming World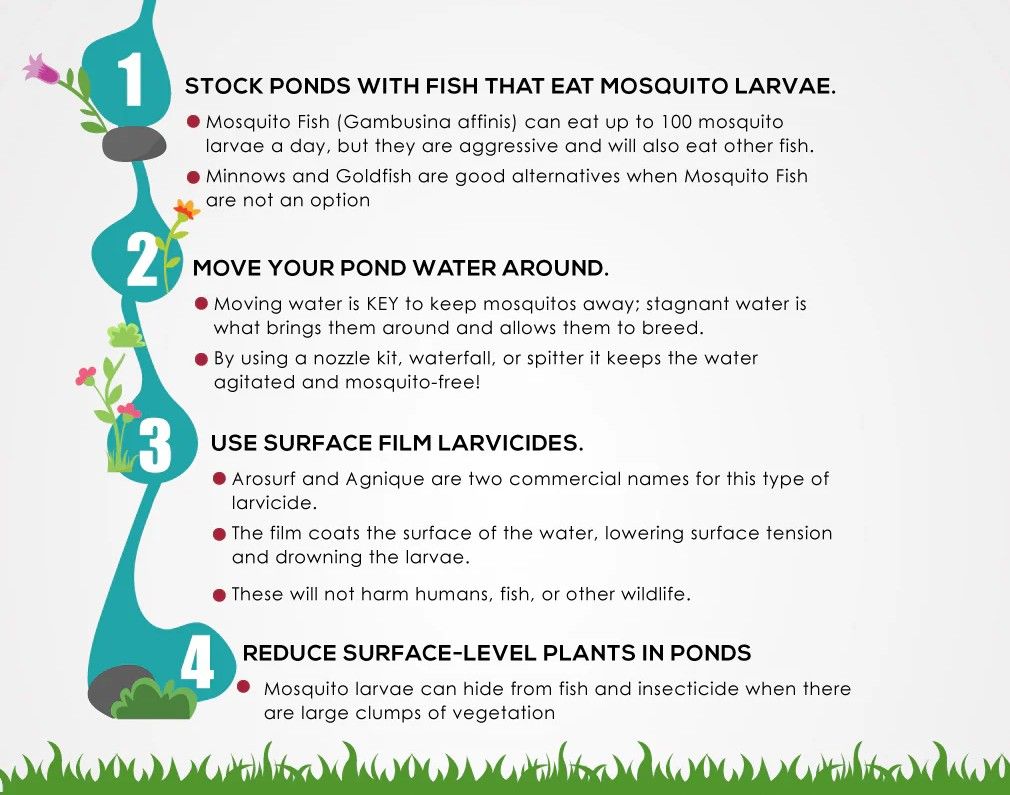
Combating Dengue requires a multi-faceted approach known as Integrated Vector Management (IVM), incorporating environmental management, biological and chemical control, personal protection, surveillance, and community engagement:
- Environmental Management (Source Reduction): The most sustainable approach involves eliminating or managing mosquito breeding sites. This requires strong community participation:
- Regularly emptying, covering, or disposing of water-holding containers (tires, buckets, pots, drains).
- Cleaning gutters, managing waste properly.
- Installing tight-fitting lids on water storage tanks.
- Chemical Control: Using insecticides, though concerns about resistance and environmental impact necessitate careful use:
- Larviciding: Treating potential breeding sites with larvicides (e.g., temephos, insect growth regulators) to kill immature mosquitoes.
- Adulticiding (Fogging): Space spraying with adulticides during outbreaks to quickly kill infected adult mosquitoes. Effectiveness can be limited and temporary. Insecticide resistance is a growing problem.
- Biological Control: Introducing natural enemies or modifying mosquitoes:
- Larvivorous Fish/Copepods: Introducing organisms that prey on larvae into certain water bodies.
- Wolbachia Bacteria: Releasing mosquitoes infected with *Wolbachia* bacteria, which reduces their ability to transmit Dengue virus. This has shown promising results in several pilot projects worldwide (World Mosquito Program).
- Sterile Insect Technique (SIT): Releasing sterilized male mosquitoes to mate with wild females, reducing overall population numbers (still largely experimental for *Aedes*).
- Personal Protection: Individual measures to avoid mosquito bites:
- Using EPA-registered insect repellents containing DEET, Picaridin, IR3535, or Oil of Lemon Eucalyptus.
- Wearing long-sleeved shirts and long pants, especially during peak biting times (*Aedes* are primarily daytime biters, particularly early morning and late afternoon).
- Using window and door screens, air conditioning, and mosquito nets (especially for infants or those sick with Dengue to prevent further spread).
- Surveillance and Response: Strong disease surveillance systems to detect outbreaks early, monitor mosquito populations and insecticide resistance, and enable rapid public health responses.
- Vaccine Development: A complex area due to the four serotypes and risk of ADE:
- Dengvaxia® (Sanofi Pasteur): Approved in several countries but primarily recommended for individuals aged 9-45 with confirmed previous Dengue infection due to increased risk of severe disease in seronegative individuals who get vaccinated.
- Qdenga® (Takeda): A newer vaccine approved in regions like the EU, UK, Brazil, and Indonesia. Designed to be suitable for individuals regardless of prior exposure, though data and recommendations continue to evolve.
- Other vaccines are in development.
- Community Engagement and Education: Empowering communities with knowledge about prevention, source reduction, recognizing symptoms, and seeking timely medical care is crucial for sustained control.
The Ultimate Lever: Climate Change Mitigation and Adaptation
While vector control and public health measures are essential for managing current outbreaks, fundamentally addressing the Dengue threat requires tackling its climate driver. Global efforts to reduce greenhouse gas emissions according to Paris Agreement targets are critical to limit further warming and associated increases in Dengue suitability. Simultaneously, adaptation strategies like climate-resilient urban planning, improved water resource management, and enhanced early warning systems based on climate forecasts are necessary to cope with the risks already locked in.
Conclusion: A Global Health Imperative in a Changing Climate
Dengue fever represents a potent example of a climate-sensitive disease whose burden is rapidly increasing due to global warming, urbanization, and mobility. Its expansion into new regions and the intensification of outbreaks in endemic areas demand urgent, coordinated action. Effective control requires not only strengthening traditional public health responses like vector control, surveillance, and clinical management but also demands robust community participation, innovation in tools like *Wolbachia* and vaccines, and, crucially, a global commitment to mitigating climate change. Failing to address these interconnected challenges will only allow Dengue's relentless advance, further straining healthcare systems and impacting millions of lives worldwide.